Plantar fasciopathy is a term used to mean pain or inflammation of your plantar fascia, a strong band of fibrous tissue that stretches from your heel to your middle foot bones.
It supports the arch of your foot and also acts as a shock absorber in your foot.
How common is plantar fasciopathy?
Common, with around 1 in 10 people getting plantar fasciopathy at some time in their life. It is most common in people between the ages of 40 to 60 years. However, it can occur at any age. It is twice as common in women as men. It is also common in athletes.
How does it occur?
Repeated small injuries to the fascia (with or without inflammation) are thought to be the cause of plantar fasciopathy. The injury is usually near to where the plantar fascia attaches to your heel bone. You are more likely to develop pain in your plantar fascia in certain situations, for example:
- If you are on your feet a lot, or if you do lots of walking, running, standing, etc, when you are not used to it – this is known as an overload mechanism
- If you lead a sedentary lifestyle and the plantar fascia is underloaded regularly
- If you have recently started exercising on a different surface, e.g. running on the road instead of on grass
- If you have been wearing shoes with poor cushioning or arch support
- If you are overweight, as this will put extra strain on your heel
- If you have a tight Achilles tendon (the big tendon at the bottom of your calf muscles above your heel). This can affect your ability to flex your ankle and make you more likely to damage your plantar fascia.
Often there is no apparent cause for plantar fasciopathy, particularly in older people. A common wrong belief is that the pain is due to a bony growth or ‘spur’ coming from the heel bone. Many people have a bony spur of the heel bone but not everyone with this gets plantar fasciitis.
What are the symptoms?
The main symptom of plantar fasciopathy is heel pain when you walk. You may also feel pain when you stand and even when you are resting.
The pain typically occurs first thing in the morning after you get out of bed, when your foot is placed flat on the floor.
The pain usually lessens with more walking, but you may have it again after periods of rest.
How is it diagnosed?
Your physiotherapist or doctor can usually diagnose plantar fasciopathy with a clinical assessment and talking with you. Imaging, e.g. ultrasound scans and MRIs are not required to make this diagnosis.
How long does it take to heal?
The plantar fascia, like tendons throughout our body, do not have a great blood supply, therefore typically take longer to heal than other soft tissue injuries, e.g. muscle strains.
It can take anywhere from a few weeks to settle down if treated appropriately, compared to a number of months for a problem that has not been treated accordingly.
How is it treated?
Relative rest is key; resting from aggravating factors, whilst attempting to keep mobile is important. Avoid high impact exercise to the heel, e.g. running, excess walking or standing, and undue stretching of the plantar fascia.
Painkillers such as paracetamol will often ease the pain. Anti-inflammatory medicines such as ibuprofen are also useful, taken orally or via topical rubs to the heel itself.
An ice pack (such as a bag of frozen peas wrapped in a tea towel) and held to your foot for 10-15 minutes may also help to relieve pain. (Do not put ice directly next to skin as it may cause ice burn.)
Try to cushion your foot. You can do this by wearing soft soled, supportive trainers, even at work.
You can buy various pads and shoe inserts to cushion the heel and support the arch of your foot. These work best if you put them in your shoes at all times. If your heel is tender, cut a small hole in the heel pad at the site of the tender spot. This means that the tender part of your heel will not touch anything inside your shoe. Place the inserts/pads in both shoes, even if you only have pain in one foot.
Lose weight if needed.
Passive treatments, such as massage and electrotherapy are not warranted.
A graded loading and strengthening exercise regime is perhaps the most important method of improving plantar fascia pain. The plantar fascia responds well to incremental loading. Under-load it (by just resting) and the plantar fascia does not adapt to any load, therefore will continue to be painful when it is asked to work. Equally, overloading it (by doing too much, too quickly) can cause pain to become exacerbated.
This can include adjunct stretching of the calf complex.
A steroid (cortisone) injection is sometimes tried after the above have been trialled and have failed. It is important to remember that whilst an injection may relieve the pain in some people for several weeks, it does not always address the cause of the problem. Steroid injections do carry some risks too, including (but rarely) infections and rupture of the plantar fascia.
Rehabilitation Exercises
Regular, gentle strengthening of the plantar fascia, combined with stretching your calf complex may help to ease your symptoms.
Also, when you are asleep overnight, your plantar fascia tends to tighten up so in the morning you could massage your foot with anti-inflammatory gel and perform a towel stretch and a frozen can roll before getting out of bed – this reduces the pain experienced when stepping out of bed first thing.
If the exercises make the pain worse then reduce the number of times you do the exercises.
If at any time your symptoms change or worsen you must stop any exercises / self-management and consult your doctor.
How long will the effects last?
You may find that the pain is sometimes worse and sometimes better over time. If you get treatment soon after you notice the pain, the symptoms should stop after several weeks. If, however, you have had plantar fasciitis for a long time, it may take many weeks to months for the pain to go away.
Plantar fasciopathy is a self-limiting problem that usually improves itself within a year, however, doing these exercises can often mean that you will get better quicker.
How can I prevent plantar fasciopathy?
There are certain things that you can do to try to prevent plantar fasciitis, especially if you have had it before.
These include:
- Regularly changing trainers used for running or walking
- Wearing shoes with good cushioning in the heels and good arch support
- Losing weight if you are overweight
- Avoiding exercising on hard surfaces
- Performing relevant strengthening exercises as part of a weekly routine.
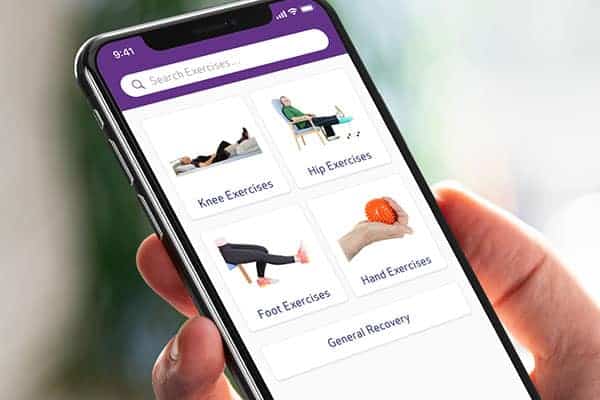
Pocket Physio | Download now
Search for ‘Pocket Physio’ on the Apple App Store for iOS and the Google Play Store for Android to download for free.




